20 Jun DEPRESSION – A BREAKDOWN IN COMMUNICATION

In recent months the subject of depression got the world’s attention when two high-profile personalities were reported to have taken their own lives.
Those of us who have had personal experiences with depression, whether ourselves or with a loved one, can attest to how such a deep sense of hopelessness can swallow someone up.
Depression is a huge subject – degrees of it, how did it start, is it mental, is it physical, which medication, which therapies, is there a “cure”, etc?
Personal and Social Factors
Difficult personal and social circumstances could be the start, building up stress, worry and anxiety that culminate to drag someone’s mental moods so low that it gets classified as depression.
Personal and social factors include:
- financial difficulties
- unresolved childhood traumas or adverse events
- unhappy relationships, family life
- grief
- stress at work
- loneliness or isolation
- low self-esteem
- lack of meaning or purpose in life
There are steps that can be taken to help with some of these root causes, some easier than others, e.g., working a payment plan or learning to manage your finances if you are in financial difficulty. If you are lonely or isolated join groups with like-minded people whether in person or online.
Lack of communication because of fear of rejection, miscommunication because there is too much chatter and not enough listening may be part of why personal and social factors seem insurmountable. There are no simple solutions and no one solution that fits everyone.
In this blog I’d like to bring attention to how such stressors impact your body systems including the brain that then manifests as the symptoms of depression.
Stress Hormones and Thyroid
Any kind of stress, whether from difficult personal situations, or internally from illnesses, infections or inflammation, trigger a system in our body to produce certain hormones to deal with the stress. This is the Hypothalamus-Pituitary-Adrenal (HPA) axis.
Any negative thought or experience is perceived by the hypothalamus in the brain which signals to the pituitary to produce its hormones. One of the pituitary hormones then signals the adrenal glands to produce stress hormones e.g. adrenaline to deal with short-term stress and cortisol for longer enduring stress.
Once there is enough stress hormones produced, a feedback mechanism tells the hypothalamus and pituitary to tone down their signals. The adrenal glands calm down and a balance is reached. However, if there’s a faulty feedback mechanism, too much or too little stress hormones, particularly cortisol, are produced and this imbalance affects moods.
Miscommunication in the HPA axis frequently affects thyroid function. There is a similar communication loop from the hypothalamus to the pituitary to the thyroid and back to the hypothalamus and pituitary. The adrenal glands and the thyroid impact each other as well, e.g. too much or too little cortisol produced by the adrenal glands affects thyroid hormones production and the balance between active and inactive thyroid hormones.
Low levels of active thyroid hormones is one of the drivers of depression.
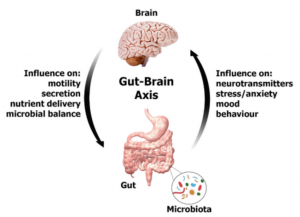
Our Second Brain
When we are stressed for whatever reason, our digestive system shuts down or reduces the production of stomach acid and digestive enzymes to devote energy to other parts of our body to “fight or flee” from a perceived enemy.
 This sub-optimal digestive system is now weaker and a very important immune system governed by the balance between the protective and harmful bacteria, yeasts, viruses in our gastrointestinal (GI) tract is compromised.
This sub-optimal digestive system is now weaker and a very important immune system governed by the balance between the protective and harmful bacteria, yeasts, viruses in our gastrointestinal (GI) tract is compromised.
Research is still uncovering the complexity of our GI tract that goes beyond dealing with digestion. It is now referred to as our second brain as it produces about 40 neurotransmitters, like the ones found in the brain, including dopamine, the “motivating neurotransmitter” and serotonin, the “happy neurotransmitter”. In fact, 90 percent of our serotonin is produced by our gut microbes.
Our gut using its own neurotransmitters communicates with the brain through the vagus nerve and can therefore alter our moods.
Worry, emotional stress or an infection or inflammation that’s affected the gut’s protective barrier or the balance of the microbiota changes the production and expression of neurotransmitters in the GI tract. Depression may then be a direct result of changes in communication between the gut and the brain.
Nutrients, Toxins, Genetics
We need adequate and the right balance of numerous nutrients for our body systems to function optimally.
E.g. low zinc and magnesium status are correlated with resistant depression and impairs our ability to detoxify toxins. Amino acids like tyrosine from protein foods are needed to make neurotransmitters and thyroid hormones. Various B vitamins, some of which are produced by our gut bacteria, are needed for adrenal function.
Modern living exposes us to more and more toxins from chemicals and heavy metals like mercury and aluminum that affect our brain function and other body systems.
Underneath all these are our genetics that is like a map of our strengths against and vulnerabilities towards expressing certain health issues. Depending on our diet, lifestyle. environmental and emotional exposures, our genes may or may not be significant to developing depression.
Untangling the Cross Talk
There is an underlying theme of a communication breakdown in depression, whether it’s in family, relationships, traumatic experiences or in our physical body systems.
Here are some tests that can help clarify what is happening in the communication within your body systems.
- A full thyroid panel that includes the active thyroid hormone, inactive thyroid hormones and antibodies.
- A comprehensive hormones test that can assess your HPA axis and your stress hormones production.
- A PCR (DNA-based) comprehensive stool test to assess your GI function and microbiota.
- Organic acids tests that reveal nutrients, neurotransmitters and toxins status.
- Genetic tests.
Self-Help Tips
- Eat a blood sugar balancing diet to help stabilize your moods. This means avoiding processed and sugary foods as much as possible. Include some protein and good quality fats in every meal.
- Use antibiotics only when absolutely necessary as they wipe out both protective and harmful gut bacteria.
- Eat as wide a diversity of vegetables as possible and legumes if tolerated. Include small amounts of fermented foods like kefirs, sauerkraut and kimchi. These promote the growth of good gut bacteria but if you have problems in the GI tract, you may experience bloating or other symptoms.
- Avoid alcohol and caffeine as they deplete nutrients.
- Get out into nature as much as possible as this calms the mind and exposure to nature such as some dirt and soil cultivates a stronger, more diverse gut microbiota.
- Avoid chemicals as much as possible such as in household cleaners and sanitisers.
Someone facing a dark night or day may find it too difficult to implement self-help tips. If possible, find a healthcare practitioner to work with or get into a support group. Reach out in whichever way possible. It can be simply hugging a pet or listening to an inspiring talk or reading a book by someone who has overcome a similar experience.